Speedier Sepsis Detection: Recent Advances in Biomaker Sensing Platforms.
- ACS BCP
- Jan 28, 2024
- 3 min read
Introduction
Sepsis is the body’s extreme response to an infection. It is a life-threatening medical emergency. It happens when an infection you already have triggers a chain reaction throughout your body. It poses a significant threat to patients in hospitals worldwide, necessitating swift and accurate diagnosis to initiate timely treatment. Most cases of sepsis start before a patient goes to the hospital. Infections that lead to sepsis most often start in the lung, urinary tract, skin, or gastrointestinal tract. In India alone, sepsis cases have been estimated to be 11.3 million, with 2.9 million deaths in 2017, as per CHEST Journal. As per CDC, at least 1.7 million adults in USA develop sepsis and at least 3,50,000 adults who develop sepsis die during their hospitalisation or are discharged to hospice.
Existing diagnostic methods often fall short due to their lack of speed, selectivity, or sensitivity. Without timely treatment, sepsis can rapidly lead to tissue damage, organ failure, and death. This gap has spurred the development of rapid sensing platforms that target biomarkers associated with sepsis. This Mini-Review explores recent advancements in biomarker sensing platforms tailored for sepsis diagnosis, focusing on their importance, the biomarkers involved, detection mechanisms, and innovations in point-of-care (POC) instruments.
Significance of Rapid Sepsis Detection
Sepsis ranks as the leading cause of in-hospital deaths globally, emphasizing the critical need for swift and reliable diagnostic techniques to initiate treatments promptly. Current clinical methods, such as the sequential organ failure assessment (SOFA) and quick SOFA (qSOFA) criteria, and blood culture tests, face challenges in accuracy, analysis time, and differentiation of patient conditions. Hence, there's a pressing need for novel sensing platforms to enhance diagnostic accuracy and efficiency.
Septic Biomakers and Detection Methods
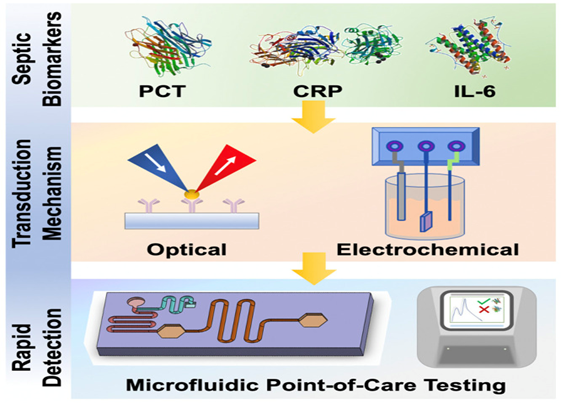
Soluble biomarkers offer a promising avenue for sepsis detection, providing faster analysis times compared to traditional blood culture methods. Key biomarkers such as CRP, PCT, and IL-6 have demonstrated clinical relevance in sepsis detection. These biomarkers are commonly detected using antibody-functionalized biosensors, with recognition events translated into quantifiable responses via electrochemical or optical methods.
Rapid Point-Of-Care Sensors for Septic Biomakers
Recent developments in electrochemical, optical, and microfluidic sensors demonstrate significant progress in reducing diagnosis time while maintaining sensitivity and specificity. Electrochemical sensors offer high sensitivity and fast analytical time, with examples like IL-6 and PCT sensors showcasing clinically relevant limits of detection within minutes. Optical sensors, including fluorescence-based assays, provide rapid results, often within an hour, with promising sensitivity for biomarker detection. Microfluidic sensors leverage miniaturization and controlled analyte flow to achieve rapid and portable diagnostic capabilities.
Recent Development
Johns Hopkins Medicine has developed TREWS (Targeted Real-time Early Warning System), an AI-driven program detecting sepsis almost six hours earlier than conventional methods. Dr. Albert Wu from Johns Hopkins Center for Health Services and Outcomes Research estimates that TREWS may have saved hundreds of lives.
TREWS analyzes vast patient data, including lab tests and vital signs, scanning for sepsis indicators. Once it identifies at-risk patients, it alerts physicians with explanations and evidence-based recommendations. A study published in Nature reported a 20% decrease in sepsis-related deaths after testing TREWS in five hospitals over two years.
Dr. Wu highlights TREWS' potential to predict other conditions like kidney or heart failure and patient deterioration post-hospitalization. Disseminated by Bayesian Health, this AI platform offers a data-driven approach for enhancing patient care across healthcare settings.
Conclusion
The potential of biomarker sensing platforms in sepsis diagnosis, offers effective advantages in speed, efficiency, and reduced sample volume compared to traditional methods. Challenges persist in balancing speed and accuracy, addressing fabrication costs, and obtaining regulatory approvals for clinical use. Multiplexed sensors capable of detecting multiple biomarkers simultaneously hold promise for enhanced diagnostic power and early intervention. Despite current limitations, ongoing advancements in sensing technologies offer hope for improved sepsis diagnosis and patient outcomes.
reference
by-KREETI MAURYA




Comments